Opinion: the CervicalCheck scandal has put a sharp focus on the quality of screening services in Ireland
By James O'Mahony, TCD
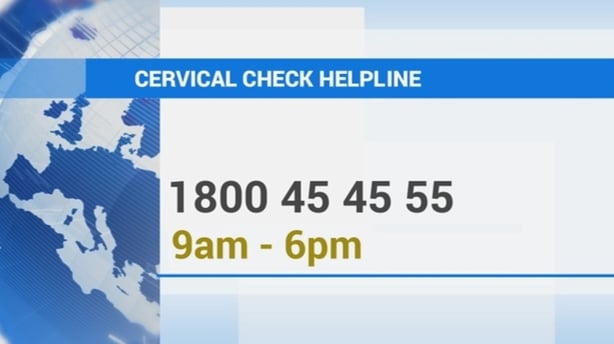
The CervicalCheck controversy has drawn attention to population screening programmes and their role in preventing cancer. Much of the coverage around cervical cancer screening revealed gaps in the understanding of screening in the minds of the public and media alike.
It is helpful to review some of the central features of cancer screening. Screening tests are applied to populations of healthy people at risk of disease. The early detection of cancer and pre-cancer can enhance the chances of survival for a number of different cancers. Population testing needs to be carefully balanced to detect as many true cases as possible without raising too many false positives. Screening also needs to be quick, convenient and affordable for it to be viable to apply on a population basis.
The types of tests used to detect disease vary from cancer to cancer and from other diseases. Generally, we attempt to spot signs of disease, ideally at its earliest stages. Most tests don't provide a simple black and white indication of cancer, but rather various shades of grey which need to be resolved with a careful additional follow-up tests.
We need your consent to load this rte-player contentWe use rte-player to manage extra content that can set cookies on your device and collect data about your activity. Please review their details and accept them to load the content.Manage Preferences
From RTÉ Radio One's Morning Ireland, Dr David Fennelly, Consultant Medical Oncologist at St Vincent's Hospital in Dublin, discusses the Scally review into the CervicalCheck controversy
Avoiding false positives in screening programmes is very important. Most people screened will be perfectly healthy and a large number of the initial positive test results will actually be false alarms that will be ruled out at the follow-up tests that are applied following a positive at a primary screening test. A screening programme that generates too many false alarms means that staff and testing resources will be consumed with conducting follow-up examinations.
The types of tests that work well for screening are not necessarily the best for diagnostic testing of people already suspected of having disease. It is acceptable to use more invasive tests that take longer to conduct in a diagnostic context. This is because there are fewer tests to conduct and the risks of false positives do not apply over the whole population.
The CervicalCheck scandal has put a sharp focus on screening service quality
No screening test is perfectly accurate at detecting disease. It is a sad inevitability that some women in a cervical screening programme will have failed to have their disease detected at an earlier stage. The fact that some cancers were not detected is not necessarily evidence that the programme was not working properly. Even a well functioning screening programme will be expected to have some false negatives. This point appears not to have been understood by many at the time the controversy erupted.
Similarly, we must recognise the fact that signs of disease that had previously been missed when previous tests were reviewed as part of an audit process do not necessarily indicate a systematic failure of services. It may be possible to detect unhealthy cervical cells that would indicate the need for further investigation when experts have the benefit both of hindsight knowing that disease did develop and more time than used during the standard screening process.
We need your consent to load this rte-player contentWe use rte-player to manage extra content that can set cookies on your device and collect data about your activity. Please review their details and accept them to load the content.Manage Preferences
From RTÉ Radio One's Ray D'Arcy Show, Lorraine Walsh, Stephen Teape and Vicky Phelan talk about Dr Gabriel Scally's report
It is natural to ask why all slides are not reviewed slowly and why is screening not conducted on a more regular basis, as is practiced in some countries. The answer is that such testing practices would be very expensive and would likely only detect a very small additional proportion of disease. The small additional health gain at large additional cost cannot be justified when we consider the alternative funding needs elsewhere in the Irish health system. Achieving an appropriate balance of service provision requires discipline to restrict current screening intensity to appropriate levels.
The CervicalCheck scandal has put a sharp focus on screening service quality. There are undoubtedly important questions to ask about the adequacy of test performance. The fact that Dr Gabriel Scally has not recommended a commission of inquiry indicates that there does not appear to be fundamental concerns regarding the quality of screening provided by the labs under review.
We need your consent to load this rte-player contentWe use rte-player to manage extra content that can set cookies on your device and collect data about your activity. Please review their details and accept them to load the content.Manage Preferences
From RTÉ Radio One's News At One, a report into Dr Gabriel Scally's report into the CervicalCheck controversy
Despite the shock of the failing of screening to prevent all cancers, it is important to keep the prospects for successful cancer prevention in perspective. Ireland's adoption of organised breast, colorectal and cervical screening represents a large step forward from our previous system of ad-hoc screening. New HPV DNA tests are anticipated to further improve cervical screening performance.
Accordingly, women who attend screening can greatly reduce their risk of disease. Indeed, we should remember that attendance at screening is the single most important driver of screening effectiveness. Furthermore, we also need the public to understand that colorectal screening remains massively under-utilised. Only about 40 percent of the population eligible to for free testing for the early detection of colorectal screening actually avail of the service. Again, the main best way to prevent cancer deaths is to increase the number people using such services in the first place.
Dr James O'Mahony is a Research Fellow in Public Health & Primary Care at Trinity College Dublin
The views expressed here are those of the author and do not represent or reflect the views of RTÉ

