Analysis: a new study has found that the health system is not helping junior doctors to recognise their role in shaping a safety culture
By Éidín Ní Shé and Eilish McAuliffe, UCD
What influences patients’ trust in health professionals? Some of the factors are clear communication, respect for autonomy and shared decision-making, maintaining confidentiality, honesty, openness and transparency. As the fallout from the Cervical Check scandal continues, the focus has now shifted on making open disclosure mandatory across the health system.
Open disclosure is defined by the HSE as "open, consistent approach to communicating with service users when things go wrong in healthcare". In the United Kingdom, open disclosure - or "duty of candor" as they term it - was introduced in April 2013 and was refined again in 2015. The update followed from the inquiry at the Mid‐Staffordshire Hospital Trust that found hundreds of patients had died needlessly due to staff failing to speak up about substandard care.
We need your consent to load this rte-player contentWe use rte-player to manage extra content that can set cookies on your device and collect data about your activity. Please review their details and accept them to load the content.Manage Preferences
From RTÉ Radio One's News At One. Justin McCarthy reports on the evidence by the Health Service Executive's John Connaghan to the Public Accounts Committee about the Cervical Check scandal
In Ireland, the Health Information and Quality Authority (2012) have emphasised the importance of a culture of quality and safety that promotes transparency, teamwork and open and effective communication. Encouraging such a culture needs to start from an understanding of the factors that make it difficult for doctors and other health professionals to be open about errors.
We undertook the Medical Professionalism in Relation to Patient Safety Study to better understand junior doctors’ reluctance to speak out when they witness unsafe care. We developed a serious board game as a novel method to prompt open and honest discussions about what really happens in practice when errors are made in patient care.

This free, open-access discussion game included real stories or accounts of errors that had occurred in the past few years. We anonymised the stories and ensured they included as many different perspectives as possible. The game was designed by a group which included medical and nursing staff, quality and safety staff, patient representative and researchers.
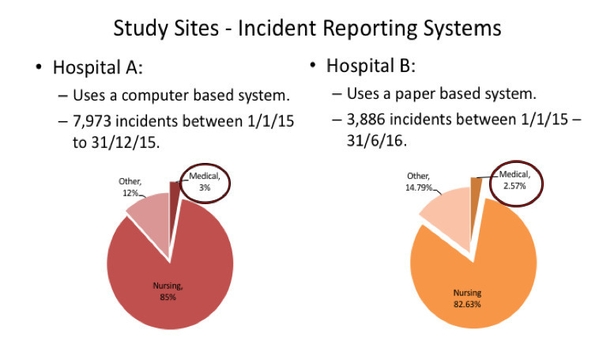
We then played the game in two hospitals comparable in terms of size and services delivered. We also collected information on the hospitals’ systems for reporting errors or incidents of unsafe care. We found that the hospital with a computerised system for reporting errors had a far higher number of errors reported than the one with a paper-based system. We also found that medical staff reported very few incidents compared to nursing staff.
A total of 101 junior doctors played the game. The use of real stories helped to open up the discussion and helped them share their reasons for not reporting patient safety errors. An additional feature of the game was to attempt to get agreement from the players about what might constitute an appropriate, workable policy on reporting errors. The overall majority (97) voted for the following statement:
"All staff should report all concerns they have regarding patient safety, without fear of recrimination, in the knowledge that learning will happen and the system will be improved. Patient safety should be our top priority as healthcare professionals."
We interviewed some of the doctors after they had played the game and this allowed us to really understand their reluctance to report errors. The junior doctors we spoke to said they were unclear of the incident reporting process and some could not recall if they had received any training. Many believed that it was a nurse’s job to report and nursing staff reported for them.
Our research found that the existing system is not supporting junior doctors to recognise their role in shaping a safety culture
Junior doctors noted that they also frequently observed nursing staff creating an enabling environment to report:
"Nurses are definitely more inclined...They would encourage each other to help each other to maybe put in the incident report form and say ‘No, that is definitively an incident you need to put that in' or 'Listen, you go put that in now and I will do your job’. They are definitely more inclined". Janet (Hospital A)
This was in contrast to a lack of visible reporting by their medical colleagues. Here's a trainee doctor commenting on lack of visible reporting behaviour in senior medical colleagues:
"From the point of my internship, I never had a Registrar or Senior House Officer or a Consultant that would tell me that they are going to report an incident or do one". Carli (Hospital B)
Many questioned why they would bother reporting, given the absence of feedback following submission of a report:
"It’s just I suppose a bit depressing, but I feel like we cannot change the system at all, that there is no point of filling out one form". Mia (Hospital B)

The junior doctors seem reluctant to report on senior colleagues:
"If there is an incident with someone more senior to you on your team, that’s when you are least likely ..to say anything...we cannot really critique people above us as a rule. It just doesn’t happen". Angelo (Hospital B)
When asked, the junior doctors said frequent feedback that would support ongoing learning would be necessary to encourage more reporting:
"People want to see the reporting loop closed when you report and seeing on outcome on that". Monika (Hospital A)
A mandatory open disclosure policy will be a welcome development in promoting safer healthcare. However in order to develop an open responsive health system, the policy will need to be supported by ongoing training and supported learning across the health system.
Our research found that the existing system is not supporting junior doctors to recognise their role in shaping a safety culture. The limited training being provided to them is seen as a token gesture resulting in a limited understanding of the purpose of reporting. Unless senior medical staff take their responsibility to reduce errors and unsafe care seriously and behave accordingly, it will be difficult to change the behaviour of more junior staff. The focus should be on developing a safety culture that is supported by education and learning - and led by the example of senior health professionals.
Dr Éidín Ní Shé is a research fellow at the School of Nursing, Midwifery and Health Systems at UCD. Professor Eilish McAuliffe is a professor of health systems at UCD and is a current Irish Research Council awardee. The Medical Professionalism in Relation to Patient Safety Study was funded by the Health Research Board Medical Education grant (2015-2017).
The views expressed here are those of the author and do not represent or reflect the views of RTÉ

