Analysis: new high impact research aims to use stem cells from patients as a method of breast reconstruction after mastectomy
Breast cancer is a global healthcare challenge, with the National Cancer Registry predicting that there will be approximately 5,000 new breast cancer cases in Ireland per annum by 2020. Despite the development of more sensitive methods of diagnosis and advances in oncological treatment, surgical excision of the tumour is still a critical part of breast cancer treatment.
40 percent of breast cancer patients require a mastectomy to treat their disease. This rate is increasing due to more patients undergoing risk-reducing mastectomies after diagnosis of genetic mutations which increase their risk of developing breast cancer, as seen in the case of Angelina Jolie in 2013. Mastectomy is a disfiguring operative procedure, and can result in significant physical and psychological issues for patients. Immediate breast reconstruction has become an integral part of breast cancer care, affording psychosocial and cosmetic benefits.
Currently, breast reconstruction is carried out by two distinct methods: (1) the insertion of a silicone implant or (2) the transfer of muscle or fat tissue from another area of the body to the chest wall to recreate the removed breast. Implant reconstructions are the most common breast reconstructive procedures carried out worldwide. Unfortunately, implant breast reconstruction is not without its limitations. These include inappropriate breast reconstruction volume and texture, infection, implant rupture, extrusion of the implant through the skin, foreign body reactions creating scar tissue around the implant (i.e. capsular contracture) and the need for implant replacement every 10 to 15 years.
The principle limitation of implant-based reconstruction is capsular contracture, which is a foreign body reaction resulting in the formation of a circumferential capsule of fibrous tissue around the implant. This can cause pain, decreased shoulder mobility and poor cosmetic and quality of life for patients. It also represents a significant economic burden as treatment requires re-operation with removal of the scar tissue capsule and implant replacement.
Adipose tissue engineering research focuses on the development of a new type of breast implant. This is composed of the patient’s own fat using tissue engineering strategies that will not generate the same foreign body reaction as silicone implants, thus solving the problem of capsular contracture.
Such autologous fat is thought to be a superior method of soft tissue augmentation due to a range of properties including its versatility and ability to integrate into the patient’s tissues. It is not rejected by the patient’s immune system, has similar physical properties to breast tissue and appears more natural than implants or autologous reconstructions. It also does not create a wound and scar elsewhere in the body as is necessary when harvesting large volumes of muscle and adipose tissue to recreate the breast mound in current methods of autologous breast reconstruction.
We need your consent to load this rte-player contentWe use rte-player to manage extra content that can set cookies on your device and collect data about your activity. Please review their details and accept them to load the content.Manage Preferences
RTÉ Western Correspondent Pat McGrath reports on research at NUI Galway on the use of stem cells to treat breast cancer
Adipose tissue engineering requires a stem cell with the capacity to differentiate or transform into mature adipocytes/fat cells. Adult stem cells are found in almost all adult tissues. Stem cells extracted from adipose tissue are becoming the gold standard cell source for tissue engineering as they hold several advantages over stem cells isolated from the bone marrow. They are harvested with less invasive procedures, they have a higher cell yield per gram of tissue, they grow faster and live longer in the laboratory setting and are capable of differentiating into several different mature cells types (e.g. adipocytes, osteocytes, myocytes, cardiomyocytes). We propose to extract fat and its stem cells from patients and reinject this as a method of breast reconstruction after mastectomy.
Recreating the breast mound post-mastectomy will require long-term maintenance of larger tissue volumes in engineered grafts which will require a suitable cell-supporting scaffold. Scaffolds allow for the growth of cells in a 3D microenvironment, more accurately mimicking the native tissue. The "ideal" scaffold is one that allows for the production of "native-like tissue", with similar physical and biochemical properties of the tissue it is replacing.
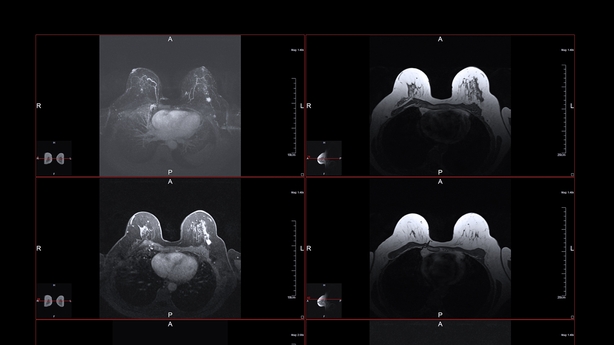
My research makes use of a scaffold known as a hydrogel, which is composed of natural proteins found within the body’s tissues and water. This provides support for stem cells and mature adipocytes and the hydrogel along with the cells it is carrying can be injected into the site of mastectomy to recreate the breast mound.
Patients will have a shorter length of hospital stay and less operating time will be spent correcting complications, thus reducing the economic burden of mastectomy
However, as this treatment will be utilised mostly by patients who have had a mastectomy for the treatment of breast cancer, assessment of the oncological safety of this strategy is central to my research. This is done by analysis of the cells used for the expression of genes known to be associated with breast cancer and by the analysis of the liquid media the cells and hydrogels are kept in for factors and chemicals known to be secreted by breast cancer or to be capable of promoting breast cancer growth or progression.
This is high impact research, funded by Breast Cancer Research, an Irish charity who raise funds for research in the field of breast cancer in NUI Galway, which aims to develop an effective reconstruction option for mastectomy patients. It overcomes the limitations of current methods of breast reconstruction and results in reduced psychosocial disease, a higher quality of life and decreased risk of requiring further reconstructive procedures due to complications.
The most significant complications we aim to overcome through the development of a new breast implant are implant rupture and capsular contracture. With this achieved, rates of reoperation will be reduced and there will be fewer hospital admissions required. Patients will have a shorter length of hospital stay and less operating time will be spent correcting complications, thus reducing the economic burden of mastectomy.
The views expressed here are those of the author and do not represent or reflect the views of RTÉ



