There have been calls for urgent action to address mental health difficulties among those experiencing homelessness.
Childhood trauma outside of the family home led Brian down a path of alcohol addiction from the age of 13.
"Gradually as the years went on, my addiction got worse and my mental health got worse," he said.
His solution to all of his problems was to run away.
A short stint in a homeless hostel in London made him realise that he had to get his life on track.
He described gaining entry to the hostel as a "degrading" experience, which required sitting in a chair to get deloused.
That was the 1970s, a time when there were not adequate supports for people coping with mental health difficulties, addiction or trauma.
It was also a time that fewer people spoke to family about their struggles.
"In later years, I found the strength to talk to my siblings, but never took the opportunity to talk to my parents about it.
"In a way, they probably went to their graves wondering why I was drinking, why I had these mental health issues...but I can live with that."
Now 19 years sober, Brian, who is a peer advocate working with people in addiction with mental health difficulties who may face homelessness, has the support of others who have been in addiction and the support of his wider family.
"My mental health has improved significantly, I still have periods where my mental health isn't good, but over the years but over the years I've developed coping mechanisms".
Report finds many homeless people struggling with depression
Brian's story comes amid calls for urgent action to address mental health difficulties among those experiencing homelessness.
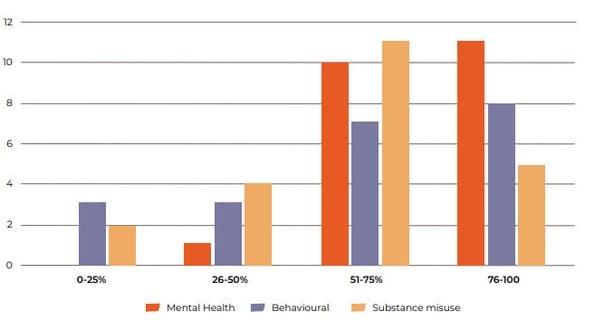
According to homeless charity Depaul, at least one in two of its residents are struggling with depression, anxiety, and suicidal thoughts.

The findings contained in a report published this morning are based on the charity's administrative data of over 4,000 individuals between 2018 and 2023.
During that time - which includes the Covid-19 pandemic - 37% of residents reported mental health difficulties.
The figure is nearly twice the national rate and more than likely underestimated, according to Depaul and Mental Health Ireland.
The report, titled 'Breaking the Cycle: Addressing Mental Health and Homelessness Through Integrated Care' has been jointly produced by both organisations.
It shows that 16% of Depaul's residents were hospitalised for mental health. That figure rose to 38% among those who self-reported mental health difficulties.
It states that current practices within community mental health teams - particularly the over-reliance on psychiatrists prescribing medications without holistic interventions - was viewed as "particularly ineffective" by service providers.
Read the full report here
Around 4% of Depaul residents have access to a psychiatric nurse, and 9% can see a counsellor.
Service providers highlighted repeated prescriptions without psychotherapy or a multidisciplinary approach, resource constraints faced by HSE teams, and the hesitancy of professionals to address mental health difficulties when addiction is also present.
"Improvements could be made with better communication and integrated care to address these systemic gaps," it states.
Participants of focus groups as part of the research also highlighted dual diagnosis as a significant barrier for people with both mental health difficulties and addiction.
This was an issue that was highlighted during the Citizen's Assembly on Drugs Use in 2023.
According to today's report, individuals are told to address their addiction before accessing mental health support, despite mental health often being the root issue.
"This creates a cycle where neither service takes responsibility, leaving individuals without help," it states.
Chief Executive of Depaul David Carroll said services need to be restructured to help people move forward successfully from homelessness.
Speaking to RTÉ's Morning Ireland, he said the majority of people Depaul helps suffer from mental health challenges, including depression and anxiety.
He said many also have complex underlying issues, such as addiction, and resources need to be pumped into the system to assist them.
Mr Carroll described the mental health system as a "major, major challenge".
"We need specific access to consult psychiatry. We need more community psychiatry nurses and we need to support our existing staff to be equipped in the best possible way to deal with what they're facing on a day-to-day basis as well," he said.
Difficulties faced by pregnant women and those in direct provision
Of the residents in Depaul supported housing who reported mental health disorders, 44.5% were female and 55.5% male.
Among men, the predominant factors contributing to homelessness were substance misuse difficulties, mental health difficulties, and family breakdowns.
Women, on the other hand, often cited domestic violence, trauma, and mental health difficulties as primary causes.
The report highlights difficulties that pregnant women in one of Depaul's housing services have faced in trying access mental health support within Dublin-based services.
Women residing at the centre faced "systemic exclusion" from healthcare providers, including primary care and mental health services, due to their homeless status.
The report has also highlighted challenges for those living in direct provision, particularly asylum seekers.
One of the outreach team members described a lack of continuity in support when people are transferred from direct provision centres to emergency accommodation, as different organisations manage services across different counties.
A significant barrier to accessing mental health services is language, particularly for residents whose first language is not English, and the availability of translators is often limited, causing delays in crisis situations.
Another concern raised in the report is the growing issue of gambling addiction and the lack of specific resources and risk assessments to address it.
One service provider pointed to the substance-focused nature of current addiction frameworks and the difficulty in finding suitable services for individuals with gambling as their primary addiction.
This was raised as a significant concern as it is "leading to people losing their tenancy and fall into homelessness".
The report recommends increased investment in staff training, support for individuals with enduring mental health issues, and targeted interventions for substance misuse and dual diagnosis care.
It says the Mental Health Bill presents "a critical opportunity" to secure the additional resources needed to address these urgent gaps in care and create a system that fully supports people experiencing homelessness.
It has called for increase access to counselling, psychiatric services, and peer-led support systems, particularly for individuals with dual diagnoses, and expand on-site mental health services to increase access and reduce delays.
Other recommendations include strengthening coordination between homelessness, addiction, and mental health services and establishing multidisciplinary teams to address clients' needs holistically.







