It is hard to think of anything more important than a child's mental health.
During these formative years, what goes on in a young person’s mind is crucial for their future development, hopefully into a happy, healthy person.
In what was perhaps her fundamental conclusion, the Inspector of Mental Health Services, Dr Susan Finnerty said that she could not currently assure parents and guardians that their children have access to a safe, effective, and evidence-based mental health service.
All children have a right to enjoy the highest attainable standard of physical and mental health under Article 24 of the United Nations Convention on the Rights of the Child, which was ratified by Ireland in 1992.
The 140-page review published by the Mental Health Commission mostly makes for grim reading.

In the past, public mental health services have often been labelled the "Cinderella" of the health system, as it has been seen as neglected, underfunded and finds it hard to compete with other major health services.
The review process published this week looked at a sample of 10% of case files in the CAMHS system. The conclusion is that CAMHS is a postcode lottery.
It seems incredible that most CAMHS services do not have an information technology system that manages patients' appointments, staff rotas, clinic files, or activity reports.
One CAMHS team was still using Windows 7. One team had no idea which cases were open or closed in their filing room.
The Inspector reveals in her report:
"We found that paper-based clinical files were usually handwritten, often illegible, frequently bulky, had loose pages, where not in chronological order, and were incomplete."
How can the performance of any system be reviewed without these basics? Internationally, many comparable countries have patient information systems and electronic records in place for years.
The problems here also resulted in a situation where in one case, a CAMHS team had "lost" 140 cases. Thankfully, these were eventually found after a search. But these types of events do not inspire confidence.

The review found that the majority of CAMHS teams monitored children and young people on attention deficit hyperactivity disorder (ADHD). Antipsychotic medication (also known as neuroleptic medication) can be used in psychosis, or other mental illnesses.
While there was no evidence that some teams were not monitoring antipsychotic medication in accordance with international standards – there are no national standards, the Inspector said.
That means that some children were taking medication without appropriate blood tests and physical monitoring that is essential when on this medication.
The HSE was given an interim report on all this late last year and the final report was published this week. The HSE says it has been acting on the issues to deal with the "deficits and shortcomings" in the CAMHS service and that there is still a body of work to do.
The HSE said that an audit of prescribing practice around the country "in the main" found no evidence of overprescribing of medication and that 95% of patients had their medication prescribed by a consultant, or in consultation with a consultant.
It also did a review of all open cases which had not had follow-up appointments in the previous six months, and of those who had been prescribed neuroleptic medication.
Out of an overall caseload of almost 20,000 children and young people, 576 open cases were identified, and all have been contacted and the HSE said it has ensured that they are receiving appropriate care.
It said it has also not identified harm caused to these patients.
Long waiting lists are a feature of CAMHS. Just yesterday, the Social Democrats published new figures showing that waiting lists have increased by up to 20% in some areas like the Cork/Kerry region.
There are now around 4,500 children waiting for CAMHS services around the country and over 1,600 waiting over six months.
Some parents may be able to afford to get mental health treatment for their child privately, others simply do not have the resources. One family told the Inspector that they had to spend €90 a week to see a private occupational therapist and were driving a round trip three hours to do so.
Some parents and young people spoke about seeing a different doctor on each visit and they had to tell their whole story over and over. Sometimes they received different diagnoses from different doctors.
Staff shortages
Serious staff shortages have also been identified by the Inspector. The vast majority of CAMHS were below the 50% of recommended staffing.
Big shortages were found in occupational therapists, social care leaders, advanced nurse practitioners, clinical nurse specialists, psychologists, speech and language therapists and social workers.
Child and adolescent mental health is a very challenging area to work in. When funding and supports are absent, that makes the environment even more difficult and potentially a risk.
We heard this week, how staff worked beyond their contracted hours, were burnt out and frustrated by not being able to provide a safe and effective service for children.
Perhaps one of the most depressing findings in the report was that some CAMHS teams told inspectors that they were frustrated to the point they did not "bother" to escalate risk regarding patients anymore, as there was no point. They pointed to a lack of audit and review of risk management as reasons.Clinical risk covers a large spectrum of risk including the risk of suicide, self-neglect, and harm to self and others.
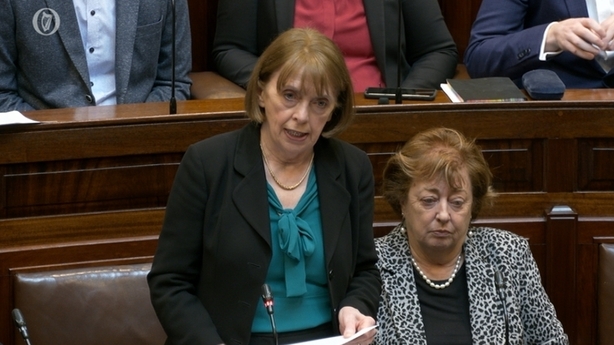
Minister of State for Mental Health & Older People, Mary Butler, said that the function of the Mental Health Commission will be expanded in the proposed new Mental Health legislation to allow the Commission to eventually regulate, register and inspect all CAMHS services.

The Mental Health Commission said that Ireland cannot wait for a new Mental Health Act given that will take time and that interim powers should be given to the Commission to act.
The Psychiatric Nurses Association described this week’s report as extremely worrying and said that it must be a final wake-up call to deal with the failings in the system.
The Irish Hospital Consultants Association also expressed major concern and said that CAMHS funding is around 0.6% of the overall health budget, amounting to it getting €125m a year.
Attention Deficit Disorder Ireland (ADDI) said there was a lack of emergency services and out-of-hours plus long waiting lists. It said that 30-50% of all children going through CAMHS are there for ADHD assessment and or treatment.
Jigsaw, the youth mental health charity, warned that the "double whammy" of a lack of funding and increasing demand is contributing to Ireland’s mental health support services being more stretched than ever before.
It pointed to Budget 2024 as an opportunity to recognise this.
Campaigners and many parents will be quite aware of the major difficulties with CAMHS, and many will not be surprised at the latest findings. That in itself is depressing.

I was at the publication in 2006 by the Government of "A Vision for Change," the new mental health policy plan for the future.
At the launch, there were promises that this landmark document would fundamentally change the way services would be delivered. Here we are 17 years later with this disturbing review report outlining today's reality.
Mental health services are a very special sector, dealing with some of the most vulnerable patients at a critical time in their developing lives. In some respects, given the nature of the delivery of mental health care, these patients are out of sight and out of mind of the general population.
People who have used CAMHS services spoke this week about how a lack of access to help can re-traumatise them. That is unacceptable.
Parents and patients who have to rely on the child and adolescent mental health services, will be hoping that this latest landmark report will be a starting point for real change and not a false dawn.
Read more: Root and branch rebuild of CAMHS needed, says Mental Health Commission chief
Settlement for boy treated by South Kerry CAMHS as family call for full public inquiry






